The Psilocybin Access Rights (#PAR) campaign’s government petition for the rescheduling of psilocybin went live on the 3rd of August 2022 and reached 10,000 signatures in under 2 months, leading the government to respond. Below, in italics, is the government response reproduced in full along with our comments on their response.
There are no plans to reschedule psilocybin to Schedule 2 of the 2001 Regulations. There is an established process for the development of medicines, including those containing Schedule 1 drugs.
The fact that psilocybin current sits in Schedule 1 is the reason the petition exists - to call on the government to make a plan to reschedule psilocybin to facilitate medical and neuroscientific research in the UK, thus facilitating the route to market authorisation and subsequent access to patients, as well as boosting life sciences research in line with the 2020 Life Sciences Sector Deal. The request would in no way amount to a queue jump to market authorisation or unrestricted access for the public, or even decreased penalties for possession, but merely a facilitation of the process of evidence collection.
The Government sympathises with patients suffering from distressing conditions and can understand the desire to seek the best possible treatment available.
The Government’s licensing regime for controlled drugs, supported by legislation, seeks to strike a balance that enables legitimate research to take place in a secure environment while ensuring that harmful drugs are not misused and do not get into the hands of criminals.
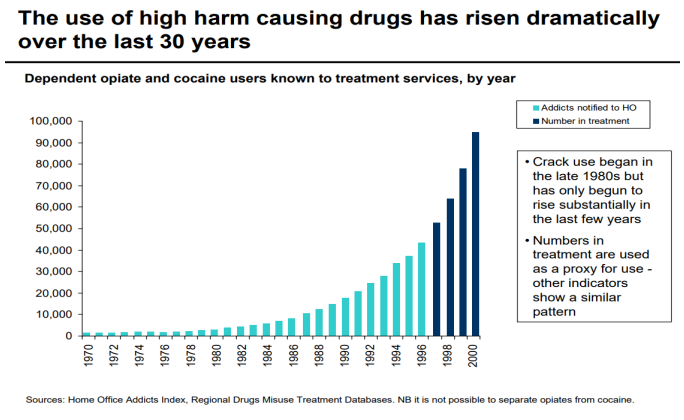
There is no evidence of users of psilocybin developing a dependency, and physiologically it is relatively safe and non-toxic - making an evidence based argument that psilocybin is a ‘harmful drug’ would be very difficult.
Compared to other controlled drugs, the proportion of the population who use psilocybin containing mushrooms is low, even though they grow wild throughout the United Kingdom. Thus psilocybin does not represent an opportunity for profit motivated gangs and criminal individuals, meaning the risk of conspiratorial diversion from research institutions is extremely unlikely. Not only that but there is no evidence of diversion of Schedule 2 substances from clinical research, even though many Schedule 2 substances, like cocaine and heroin, are of more potential harm and represent more lucrative market sizes and profit motives for criminal gangs.
The negligible criminal issue of psilocybin can be demonstrated with data from a number of FOI requests and statements from police chiefs across the country. Preliminary findings indicate that offences filed that included reference to the term ‘psilocybin’ or ‘magic mushrooms’ amounted to an average of around 12 offences per year nationally between 2015 and 2020. Thus crime which implicates psilocybin, or psilocybin containing mushrooms, accounts for only around 0.04% of all Drug Law Offences in the UK over that time period.
When we consider psilocybin’s low potential for personal and societal harm, the statistically miniscule criminal problem it represents, and the fact that there is no evidence of diversion of Schedule 2 substances, the Government’s concern is shown to be unfounded to a point at which it verges on absurd. In the light of this information, their response reads as a pronouncement made in the absence of any meaningful engagement with the evidence or the specifics of the situation regarding psilocybin.
A number of studies into the use of psilocybin as part of the treatment for mental health conditions have been or are being conducted in the UK. However, psilocybin has not yet been granted a marketing authorisation (product licence) by the Medicines and Healthcare Products Regulatory Agency (MHRA) for use as a medicine.
Psilocybin has potential as a treatment for a plethora of mental health and medical conditions, yet many proposed trials, which could address a huge unmet clinical need both in the UK and globally, fall by the wayside due to the extended time frames, increased costs, and prohibitive stigma associated with researching controlled drugs in Schedule 1.
The argument that a substance’s Schedule 1 status does not inhibit research is unfounded. This can be seen to have been acknowledged by the Government by the fact that the ACMD has been commissioned multiple times since 2017 to investigate the barriers to researching Schedule 1 drugs but has failed to move to facilitate it. While research into Schedule 1 drugs is in theory possible, in practice a tiny fraction of the possible research into psilocybin actually takes place. The first neuroscientific study in the UK in decades, published in 2012 by Prof David Nutt and Dr Robin Carhart-Harris, took several years and hundreds of thousands of pounds to be completed even though psilocybin was administered to only 15 participants - this has been acknowledged as a direct result of psilocybin’s current scheduling.
This kind smaller scale (compared to the larger Phase 1, 2 and 3 trials necessary for market authorisation) neuropsychopharmacological and other related research is massively hindered by the same barriers of cost, duration and stigma incurred by psilocybin’s unjustifiable Schedule 1 status, to the point that many interested academics are deterred from these lines of research entirely. The current status of psilocybin as Schedule 1 is obstructing research and the furthering of human knowledge without reason.
There is an established process for the development of medicines, overseen by the MHRA, which enables medicines (including those containing Schedule 1 controlled drugs such as psilocybin) to be developed, evaluated in clinical trials and licensed based on an assessment of their safety, quality and efficacy before being made available to patients in the UK. The MHRA supports the safe and scientifically sound conduct of trials in this area and also provides regulatory and scientific advice to companies at all stages of developing medicines. Should an application be submitted for a marketing authorisation (product licence), it will ultimately be a decision for the MHRA whether to license psilocybin as a therapy.
The road to licensed Market Authorisation for medicines in the UK is designed to protect the public, it is world class and should be acknowledged as such, but this is irrelevant to the request made by the petition for the rescheduling of psilocybin. Psilocybin was placed in Class A of the Misuse of Drugs Act 1971 and Schedule 1 of the Misuse of Drugs Regulations 2001 on the basis of no evidence, and no review of the evidence has ever been conducted as acknowledged in a home office response to a recent parliamentary question (UIN 61994, tabled on 12 October 2022 by Owen Thompson MP). This means that the barriers to researching psilocybin in the UK are not evidence based and are thus unjustifiable. In other words the current Scheduling of psilocybin means that there are barriers to collecting the evidence that could result in an application to the MHRA for market authorisation, which then would then potentially lead to its rescheduling, this would then facilitate the research that could lead to its market authorisation and study - which would be great had it not already been conducted… This road to rescheduling would be far too late for the UK life sciences sector and public to benefit. This obvious catch 22 is the reason the petition and the campaign for Psilocybin Access Rights exists.
If a psilocybin-based medicine is made available following an assessment by the MHRA, the Government will seek and then consider advice from the Advisory Council on the Misuse of Drugs (ACMD) on its scheduling under the Misuse of Drugs Regulations 2001. Such advice is a statutory requirement and will be considered before any decision can be taken on scheduling under the 2001 Regulations.
There is no clear reason for the Government to wait until a product has reached market authorisation to consult the ACMD on the current scheduling of psilocybin, and there is precedent for rescheduling prior to market authorisation in the case of Cannabis based products for medical use (CBPMs) which were rescheduled in 2018. This is the course of action that should be taken by the Government, for the good of the public, as has been suggested to them repetitively and consistently by numerous cross party members of parliament over the last three years.
Research into psilocybin, the active chemical in magic mushrooms, is being hindered by its Schedule 1 status under the Misuse of Drugs Regulations 2001. This status is incommensurate with the emerging evidence of its utility and relative harms, which did not exist and so was unable to inform its initial scheduling, and is affecting the growth of the UK life sciences sector. International and domestic laws on controlled substances are designed to be flexible and responsive to the evidence, yet no review of the evidence for psilocybin’s scheduling has ever been conducted, meaning after 50 years it remains in the most tightly controlled schedule without rationale.
We continue to encourage the Home Office to commission the ACMD to review the evidence with a view to rescheduling psilocybin, with restrictions to mitigate inappropriate prescribing, at the earliest possible opportunity.












.png)

--CDPRG-Side-event-05OCT2021.png)